As we all now know (unless we've been living under a rock) the only way of defeating a pandemic is to achieve 'herd immunity' for the community at large; while strictly quarantining the most vulnerable.
Herd immunity can be achieved by most people in a community catching a virus and suffering the consequences or by vaccination.
It's over two centuries since Edward Jenner used cowpox to 'vaccinate' (from 'vacca' - Latin for cow) against smallpox. Since then medical science has been developing ways to pre-warn our immune systems of potentially harmful viruses using 'vaccines'.
In the last fifty years herd immunity has successfully been achieved against many viruses using vaccination and the race is on to achieve the same against SARS-CoV-2 (Covid-19).
Developing; manufacturing; and distributing a vaccine is at the leading edge of our scientific capabilities and knowledge and is a highly skilled; technologically advanced; and expensive undertaking. Yet the rewards are potentially great, when the economic and societal consequences of the current pandemic are dire and governments around the world are desperate for a solution.
So elite researchers on every continent have joined the race with 51 vaccines now in clinical trials on humans and at least 75 in preclinical trials on animals.
Viruses, unlike bacteria or other 'germs', reproduce by taking over the reproductive mechanisms of the cells they have evolved to infect. All reproducing cellular beings like: plants, animals and bacteria are potential hosts to viruses. Thus, complex multi-cellular life-forms, like humans and other animals, have evolved strategies for dealing with them. In our case, one of these is our immune system, that once exposed to a particular virus, develops antibodies against it.
As a result of the way they reproduce, virions (virus particles) are clones of the parent virion. Their survival strategy is to be short lived but very prolific. They are therefore subject to frequent variation as a result of copying errors. Those with errors that destroy their effectiveness simply fail to reproduce but those with errors that enhance their performance become more prolific. Occasionally these variations, serendipitously, allow a virus to exploit a new host cell altogether and sometimes to jump to a new species of animal, plant or bacteria. For more on viruses read The Chemistry of Life on this website.
Yet virions are so small that they remained unseen and misunderstood until the first electron microscopes were able to resolve them in the 1930's and it would be another decade before the first safe and effective influenza vaccine would be developed - in 1942. From that time on, novel strains of influenza have become less deadly.
So it's a century since the 'Spanish Flu' killed up to 1% of the world's population. For example, due to regular immunization, influenza kills less than a thousand people in Australia, in a typical year, compared to fifteen times that number in 1919, when the population was just over a fifth of today's.
Recently revised figures put deaths due to the 1918 Spanish Flu in the United States at approximately 675,000, when the population was less than a third of today's. Thus the US death rate is now estimated to have been about 0.65% of the total population. But the US got off lightly compared to some less wealthy and organised countries.
Australia did better than most with about half the US death rate. As a result of prompt quarantine and opposite seasons, the Spanish Flu was delayed until 1919 and was then controlled by closed State borders; social distancing; and lockdowns. History repeats itself.
In the 1950's, when I was in Primary School, we were still finding our way. Indeed almost all vaccines against viruses that our grandchildren are routinely vaccinated against did not exist when I was a child.
My most memorable vaccination was after lining up at the Thornleigh School of Arts with the other kids from our school in 1955/56 to receive the first of four Salk Vaccine injections against polio. It was quite traumatic as I was once terrified of needles.
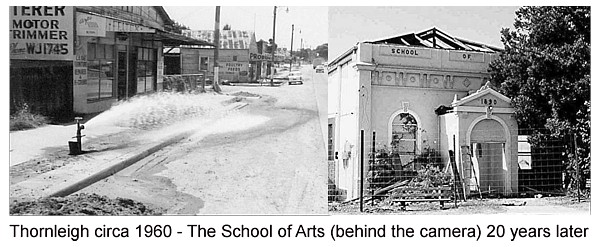
Thornleigh has changed somewhat since 1955. Both our school (up the hill in the distance in the 1960 photo - above left) and the School of Arts (once on the right side of the road, about 100 metres behind the camera) are long gone.
Polio had been running rampant around the world and several children at school wore leg callipers or had died as a result. The treatment could involve weeks in an 'Iron Lung' respirator/ventilator.
These days the common viruses that most of us of my vintage once caught like: chicken pox; mumps; and rubella; are rare in vaccinated communities.
Many viruses do not cause serious disease and some, like those that infect bacteria, may even be helpful. In others, like the highly infectious common cold, the harmful effects are slight and the costs to the community do not warrant the costs of regularly developing; testing and deploying a new vaccine.
As we have done with polio, measles, mumps and so on, herd immunity has been achieved by vaccinating a significant proportion of the population.
In the case of measles, that is very infectious, around 90% of the population need to have been vaccinated or to have caught the disease. Some other viruses are unable to spread if just half the population has antibodies, as a result of a previous infection or a vaccination. We still do not know the proportion of the population that will need to have antibodies to prevent the spread of SARS-CoV-2 (Covid-19) but it's in the range 50-70 %.
If we reduce the infection rate sufficiently, worldwide, we can effectively eradicate the virus, as we eventually did with smallpox - after two centuries of effort.
Now our scientific knowledge has advanced to the point that researchers can disassemble a virion. Yet we have become more cautious when developing vaccines as we also better understand the risks that are inherent in overstimulating our immune response; and the natural variability in response between people. The first three rules of vaccine development are test; test; and test again - a process that typically takes several to many years.
|
The Vaccine Testing Process PRECLINICAL TESTING: Potential vaccines are first tested on cells and then given to animals, typically mice or monkeys to see if an immune response results. PHASE 1 SAFETY TRIALS: The vaccine is given to a small number of people to test for safety and dosage and to confirm that it stimulates the immune system. PHASE 2 EXPANDED TRIALS: The vaccine is tried on hundreds of diverse people to see if the vaccine acts differently in them. PHASE 3 EFFICACY TRIALS: Thousands of people are vaccinated in double-blind trials (comparing the vaccine to a placebo) to see how many in each group become infected. The US Federal Drug Administration has ruled that a vaccine needs to protect at least 50% of vaccinated people to be considered effective. Phase 3 trials need to be large enough to reveal rare side effects that might have been missed in stages 1 and 2. APPROVAL: Regulators in each country review the trial results and decide whether to approve the vaccine or not. During a pandemic, a vaccine may receive emergency use authorization before getting formal approval. EARLY OR LIMITED APPROVAL: Both China and Russia have given limited approval to vaccines without waiting for the results of Phase 3 trials. As a result the efficacy (do they actually work and to what extent) is unproven and these do not yet have the required WHO accreditation or international licences to progress to mass distribution. Even though a vaccine is licensed, health systems continue to monitor it, to confirm that it’s both safe and effective. Source: The New York Times (abridged and augmented) |
The Phase 3 trial of one leading candidate, the Oxford-AstraZeneca vaccine, was briefly put on hold because of a potentially serious side effect in one volunteer that required further investigation. No doubt other candidates will suffer similar delays.
The frequent genetic variations that viruses undergo are another potential problem for vaccine designers - as most of us know from seasonal influenza, that requires a modified vaccine to be developed for new strains every year. And when a virus becomes a pandemic other problems arise.
Covid-19 has had a number of separate outbreaks and in each geographical area it has evolved in different directions resulting in a number of different strains. At least one person has caught two different strains that appear to have already diverged sufficiently so that he was not immune to the second strain when exposed. This is not good news for vaccine developers. But the better news is that, although potentially infectious, he was not ill the second time. On the other hand, this ever-changing genome is useful to contact tracers who now regularly identify the source of each infection by strain, enabling the identification of a leak in quarantine or travel restrictions to the source country or region.
The present race for a vaccine began in January 2020 but there is some evidence that the virus was circulation at a low level for months before the first identified outbreak.
In December 2019 a Chinese doctor had noticed patients suffering from a viral disease circulating in the wet markets in the City of Wuhan and initially thought it was a fresh outbreak of SARS (severe acute respiratory syndrome). As a result the markets were closed on January 1 2020. By January 5 SARS was ruled out.
On January 7 Chinese researchers warned the World Health Organisation (WHO) that they had identified a new virus named 2019-nCoV. The same day WHO warned relevant health authorities around the World.
The Chinese simultaneously provided the full genome of the virus to the world's principal reference laboratories including the US-CDC's Respiratory Viruses Diagnostic Laboratory in Atlanta; the Japanese Nagasaki Institute of Tropical Medicine and the Australian Infectious Diseases Reference Laboratory in Melbourne.
This research and the genomic information was also published in Nature on February 3 2020 (Read here...) and was a starting point for the development of both tests for the virus and for the development of vaccines. The paper has been accessed 412,000 times and has been cited 974 times by subsequent researchers some of whom have disassembled the virus down to its continent proteins and RNA.
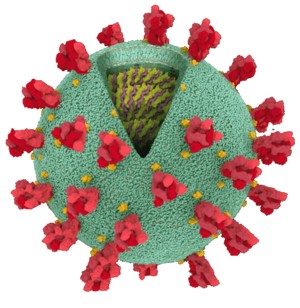 The New York Times has published a detailed map of the virus explaining its building blocks and their function.
The New York Times has published a detailed map of the virus explaining its building blocks and their function.
To read this click on the above image or go to the attachment below.
The initial goal of a vaccine is to stimulate the immune system, in trial volunteers, to produce effective antibodies against the virus, without producing serious side effects. The vaccine candidate can then be deployed to see if it prevents disease (the adverse symptoms) and/or prevents infection (spread).
There are several current approaches to developing a SARS-CoV-2 vaccine. Again from The New York Times (abridged and augmented)
- Genetic Vaccines: use one or more of the virus’s own genes to provoke an immune response.
There are at least a dozen of these in development, two of which have reached Phase 3 testing (see The Vaccine Testing Process above).
Perhaps the leading contender is the Moderna - National Institutes of Health vaccine. The US Government has already invested nearly $1 billion and awarded the company an additional $1.5 billion in exchange for 100 million doses if the vaccine proves safe and effective. Japan has made a similar deal with Moderna for 120 million doses.
Another contender is the German company BioNTech in collaboration with with US based Pfizer and the Chinese drug maker Fosun Pharma. It's now also in Phase 3, with tens of thousands of volunteers in the United States, Argentina, Brazil, and Germany. The US has awarded a $1.9 billion contract for 100 million doses, to be delivered by December, and has the option to acquire 500 million more doses.
[December addendum: The Pfizer / BoiNTech vaccine is 'first off the rank' having been given emergency approval in the UK and then the US, with Moderna not far behind. Australia has secured 10 million doses, that will be manufactured offshore, to be delivered from early 2021]
- Viral Vector Vaccines: use another virus to deliver Covid-19 genes into cells. The cells make viral proteins, provoking an immune response, but the virus cannot replicate.
At least eight teams are developing variations of these vaccines. Two are already being widely deployed in Phase 3.
The Chinese CanSino Biologics vaccine is being deployed within the Chinese Military and trialled in Saudi Arabia and Pakistan.
The Russian Gamaleya Research Institute vaccine, renamed Sputnik V, by President Putin (Warp Speed was already taken), is being trialled in Phase 3 with 40,000 volunteers. Initial (Phase 1/2) trial results have been published in The Lancet and the vaccine is expected to be licensed by December.
The Swedish-British drug maker AstraZeneca has partnered with the University of Oxford in a vaccine, that has attracted the Australian Government interest, and has also reached Phase 3. The Serum Institute of India (SII) is manufacturing the millions of doses required for the trials.
[December addendum: The University of Oxford / AstraZeneca vaccine is close to final approval and the Australian company CSL began local manufacturing on behalf of AstraZeneca at the beginning of November. Australia has secured 53.8 million doses of this vaccine - sufficient to immunise the entire population. 3.8 million doses will be delivered to Australia in early 2021. 50 million doses will be manufactured in Australia in monthly batches. Sputnik V also has emergency approval in Russia and is being distributed in several countries.]
- Protein-Based Vaccines: use a Covid-19 protein or a protein fragment (like a Covid-19 spike) to provoke an immune response.
This is the approach with the greatest number of starters but none has yet reached Phase 3 trials.
Among these is the University of Queensland, CEPI (a predominantly European consortium) and CSL (Australia) vaccine.
The US based company Novavax may be closest and has also signed a deal with the Serum Institute of India (SII) to supply Covid-19 vaccines for Phase 3 trials, about to begin in October.
[December addendum: The University of Queensland vaccine has been withdrawn due to spurious antibody production in some volunteers]
- Whole-Virus Vaccines: use weakened or inactivated Covid-19 virus to provoke an immune response.
This approach is well tried, for example against polio (Salk) and influenza, but not against coronaviruses.
Perhaps a dozen teams are working to develop a whole-virus vaccine.
Several of these are in China and three of these have reached Phase 3 testing, one of which is already approved for limited use and is being deployed in Brazil (with around 300,00 active cases) and Indonesia (28,000 and growing). As in Australia it is difficult to test for efficacy in China that presently has less than 100 active cases, insufficient exposure for a full double-blind trial into efficacy.
In addition, it's possible that vaccines already developed for other diseases may provide some protection against Covid-19. The Murdoch Children’s Research Institute in Victoria is conducting a Phase 3 trial called the BRACE to see if the Bacille Calmette-Guérin (BCG) vaccine reduces the severity of Covid-19 in Australian healthcare workers. The well established and proven to be safe vaccine is designed to protect against tuberculosis (TB). However it also boosts immunity to protect against other infections and a BCG vaccination may protect workers against Covid-19 to a, as yet undetermined, degree.
Developing and testing a vaccine is the first challenge. Then comes manufacturing; packaging; distributing; and the vaccination challenges.
[December addendum: A paragraph relating to possible Australian manufacture has been removed as it has been superseded by actual events at CSL]
The Serum Institute of India (SII), the world's largest vaccine manufacturer (by number of doses produced), is perhaps best placed to manufacture a wide range of vaccines in volume as it already produces up to 60% of the world's vaccines for Polio, Diphtheria, Tetanus, Pertussis, Hib, BCG, r-Hepatitis B, Measles, Mumps and Rubella and has a deal with the Bill & Melinda Gates Foundation to support the SII to manufacture potential vaccine candidates at maximum US$3 per dose, for distribution to to 92 impoverished countries.
In April 2020 President Trump in the US announced 'Operation Warp Speed', a White House initiative to invest billions of dollars in the development of drugs, diagnostics and treatments to combat Covid-19, including the fast-tracking of vaccines. The preferred method appears to be to pre-purchase hundreds of millions of doses of selected vaccines promising to: Make America Well Again.
Elsewhere, first-world countries are making similar provisions. But this is a pandemic and we can't halt this virus if it's running rampant in the third-world, so a bit of enlightened self-interest is called for.
On balance it appears that with any luck many of us should be lining up for a jab, just as I did back in 1955, in the middle of 2021.
In the meantime, we mere consumers must continue to wait for a vaccine and attempt to stay safe.
Finally there is some good news in Australia. As a result of social distancing and a greater uptake in flu vaccinations, this year, Covid-19 and influenza combined have killed less than does seasonal influenza alone in a typical year. This could have been significantly better had it not been for of breaches in Covid-19 quarantine in Victoria and subsequent mistakes: from which 89% of all Australian Covid-19 deaths have resulted. Yet at last Victoria seems to have got it back under control. So we are leaning and getting better at this.
